Autoimmune blistering diseases like Bullous Pemphigoid and Pemphigus Vulgaris are rare but serious conditions affecting the skin and mucous membranes. While they share similarities, they differ in their underlying mechanisms, clinical presentations, and treatment approaches. These conditions, comparing their features and highlighting the best treatment options available.
Understanding Bullous Pemphigoid and Pemphigus Vulgaris
What is Bullous Pemphigoid?
Bullous pemphigoid is a rare autoimmune disorder that primarily affects the skin, causing large, fluid-filled blisters. This condition often develops in older adults, typically over the age of 60, and can be chronic or episodic. The blisters are usually located on areas of the skin that experience frequent friction, such as the abdomen, arms, legs, and groin. While it is not life-threatening, the condition can significantly impact the quality of life due to discomfort and itching.
Related Articles: Bullous Pemphigoid – Autoimmune Skin Disorder
Causes and Risk Factors
Bullous pemphigoid occurs when the immune system mistakenly attacks the thin layer of tissue that connects the skin’s outer layer (epidermis) to its deeper layers (dermis). This attack results in inflammation and the formation of blisters. The exact cause of this immune response is unknown, but certain factors may trigger or worsen the condition:
- Medications: Drugs such as diuretics, antibiotics, and certain anti-inflammatory medications have been linked to triggering bullous pemphigoid.
- Infections: Viral or bacterial infections may act as triggers in susceptible individuals.
- Chronic Conditions: Conditions like diabetes, multiple sclerosis, or other autoimmune diseases may increase the risk.
- Age: Older adults are significantly more likely to develop this condition.

Symptoms
The primary symptoms of bullous pemphigoid include:
- Blisters: Large, tense blisters filled with clear fluid. These blisters are not prone to breaking easily.
- Itching and Redness: Intense itching often precedes the appearance of blisters.
- Inflamed Skin: The skin around the blisters may appear red or irritated.
- Mucous Membrane Involvement: In some cases, the condition can affect the mucous membranes in the mouth, eyes, or genitals, leading to painful sores.
What is Pemphigus Vulgaris?
Pemphigus vulgaris is a rare, chronic autoimmune disease that primarily affects the skin and mucous membranes. This condition is characterized by the formation of painful blisters and erosions, resulting from the immune system attacking the cells that hold skin layers together. Without prompt treatment, pemphigus vulgaris can lead to serious complications, making early recognition and management critical.
Causes of Pemphigus Vulgaris
Pemphigus vulgaris occurs when the body’s immune system mistakenly produces antibodies that target desmogleins—proteins essential for cell adhesion in the skin and mucosa. This leads to the breakdown of the bonds between cells, causing the layers of the skin to separate and form blisters.
While the exact cause of this autoimmune response is unknown, certain factors may increase the risk:
- Genetics: A family history of autoimmune diseases can predispose individuals to pemphigus vulgaris.
- Medications: Drugs such as penicillamine or certain blood pressure medications may trigger symptoms.
- Environmental Factors: Stress, infections, or trauma to the skin may contribute.

Symptoms of Pemphigus Vulgaris
The hallmark symptom of pemphigus vulgaris is the appearance of blisters and sores. These can vary in severity and typically manifest in the following areas:
- Mouth: Painful sores are often the first symptom, making it difficult to eat or drink.
- Skin: Blisters appear on the scalp, face, chest, or back and may ooze or crust over.
- Genital and Other Mucous Membranes: Less commonly, the disease affects the genital area, throat, or eyes.
Blisters caused by pemphigus vulgaris are fragile and may rupture easily, leading to open wounds prone to infection.
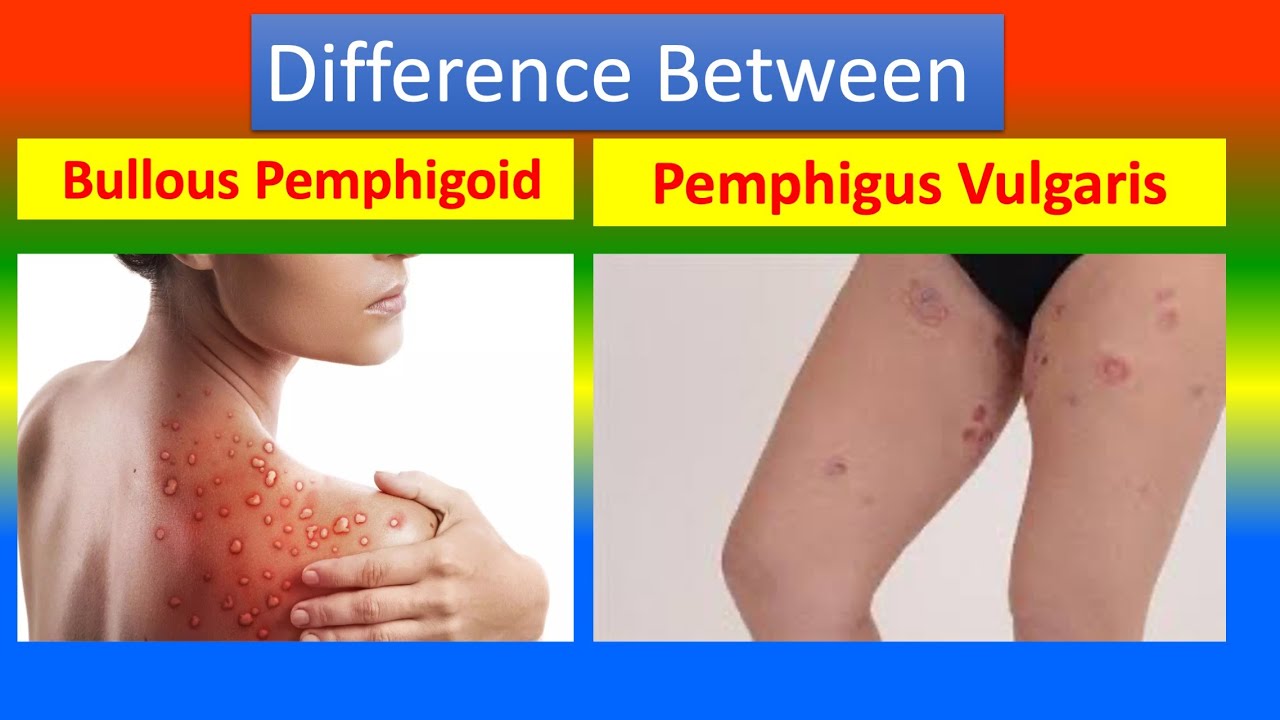
Key Differences Between Bullous Pemphigoid and Pemphigus Vulgaris
| Feature | Bullous Pemphigoid | Pemphigus Vulgaris |
| Blister Type | Tense, fluid-filled blisters | Fragile, easily ruptured blisters |
| Location | Mostly skin | Mucous membranes and skin |
| Age Group | Elderly | Middle-aged adults |
| Pathophysiology | Autoantibodies against basement membrane proteins | Autoantibodies against desmogleins |
| Prognosis | Better with treatment | Requires aggressive management |
Treatment Options for Bullous Pemphigoid and Pemphigus Vulgaris
Effective Treatments depends on early diagnosis and tailored therapies. Here are the key treatments strategies:
Related Articles: 8 Natural Remedies for Bullous Pemphigoid
1. Corticosteroids
Both conditions respond well to corticosteroids, which reduce inflammation and suppress the immune response.
- For Bullous Pemphigoid: Topical steroids like clobetasol are often sufficient for localized cases. In severe cases, systemic steroids such as prednisone may be required.
- For Pemphigus Vulgaris: Systemic corticosteroids are the mainstay, as this condition tends to be more aggressive.
2. Immunosuppressants
Medications like azathioprine, mycophenolate mofetil, or methotrexate are often used as steroid-sparing agents to reduce long-term side effects.
- Bullous Pemphigoid: Immunosuppressants are typically added in severe or refractory cases.
- Pemphigus Vulgaris: These agents are crucial for long-term disease control.
3. Biologic Therapies
Biologics targeting specific components of the immune system have revolutionized treatment.
- Rituximab: This monoclonal antibody depletes B-cells and has shown excellent results in Pemphigus Vulgaris, even achieving remission in many cases.
- For Bullous Pemphigoid: Ongoing research explores the use of biologics, but options like rituximab are used in refractory cases.
4. Antibiotics and Anti-inflammatory Agents
For Bullous Pemphigoid, tetracyclines combined with nicotinamide can be an effective alternative for mild to moderate disease.
Related Articles: Bullous Pemphigoid Natural Treatment and Some Food Avoid
5. Intravenous Immunoglobulin (IVIG)
IVIG is used in severe or treatment-resistant cases of both diseases to modulate the immune system.
6. Plasmapheresis
This technique is more commonly used in Pemphigus Vulgaris, especially for life-threatening cases. It removes autoantibodies from the bloodstream, offering temporary relief.
Supportive Care and Lifestyle Adjustments
- For Both Conditions:
- Maintain proper wound care to prevent secondary infections.
- Follow a healthy diet to support overall immune health.
- Avoid triggers like certain medications or stress.
- Specific to Pemphigus Vulgaris:
- Use oral care products designed for sensitive mouths.
- Eat soft foods to minimize irritation.
Conclusion
Both Bullous Pemphigoid and Pemphigus Vulgaris require timely intervention to prevent complications. Advances in biologics and immunosuppressive therapies have improved outcomes significantly. If you or someone you know experiences persistent blisters or sores, consult a dermatologist promptly for diagnosis and personalized treatment. Understanding these conditions is the first step toward effective management and improved quality of life.